Hyperbaric Autism Treatment
Medical Hypotheses (2006) 67, 216–228
Hyperbaric oxygen therapy may improve symptoms in autistic children
Daniel A. Rossignol a,b,*, Lanier W. Rossignol
a Blue Ridge Medical Center, 4038 Thomas Nelson Highway, Arrington, VA 22922, USA b University of Virginia, P.O. Box 800729, Charlottesville, VA, USA
Received 26 January 2006; accepted 7 February 2006
Summary Autism is a neurodevelopmental disorder that currently affects as many as 1 out of 166 children in the United States. Recent research has discovered that some autistic individuals have decreased cerebral perfusion, evidence of neuroinflammation, and increased markers of oxidative stress. Multiple independent single photon emission computed tomography (SPECT) and positron emission tomography (PET) research studies have revealed hypoperfusion to several areas of the autistic brain, most notably the temporal regions and areas specifically related to language comprehension and auditory processing. Several studies show that diminished blood flow to these areas correlates with many of the clinical features associated with autism including repetitive, self-stimulatory and stereotypical behaviors, and impairments in communication, sensory perception, and social interaction. Hyperbaric oxygen therapy (HBOT) has been used with clinical success in several cerebral hypoperfusion syndromes including cerebral palsy, fetal alcohol syndrome, closed head injury, and stroke. HBOT can compensate for decreased blood flow by increasing the oxygen content of plasma and body tissues and can even normalize oxygen levels in ischemic tissue. In addition, animal studies have shown that HBOT has potent anti-inflammatory effects and reduces oxidative stress. Furthermore, recent evidence demonstrates that HBOT mobilizes stem cells from human bone marrow, which may aid recovery in neurodegenerative diseases. Based upon these findings, it is hypothesized that HBOT will improve symptoms in autistic individuals. A retrospective case series is presented that supports this hypothesis.
��c 2006 Elsevier Ltd. All rights reserved.
Abbreviations: SPECT, single photon emission computed tomography; PET, positron emission tomography; HBOT, hyp- erbaric oxygen therapy; MRI, magnetic resonance imaging; ATA, atmosphere absolute; CP, cerebral palsy; SOD, superox- ide dismutase.
* Corresponding author. Tel.: +1 434 263 4000; fax: +1 434 263 4160.
E-mail addresses: [email protected] (D.A. Rossignol), [email protected] (L.W. Rossignol).
Background
Overview of autism
Autism is a neurodevelopmental disorder currently affecting as many as 1 out of 166 children in the United States [1] that is characterized by impair- ments in social interaction, difficulty with commu- nication, and restrictive and repetitive behaviors [2]. It affects children from all socioeconomic and ethnic backgrounds [3]. Autism was considered
0306-9877/$- see front matter ��c 2006 Elsevier Ltd. All rights reserved. doi:10.1016/j.mehy.2006.02.009
Hyperbaric oxygen therapy may improve symptoms in autistic children 217
a rare condition before the 1990’s with a preva- lence of approximately 1 in 2500 children [4]. How- ever, according to the US Department of Developmental Services, the prevalence of autism spectrum disorders increased 556% from 1991 to 1997 [5]. Autism is now more common than child- hood cancer, cerebral palsy, Down’s syndrome, spina bifida, or cystic fibrosis [6,7]. In addition, autism is found throughout the globe and the prev- alence worldwide is increasing 3.8% per year [8]. Autism is an incompletely understood disorder [3,5], but new clinical research is beginning to un- ravel some of its mysteries.
Overview of hyperbaric oxygen therapy
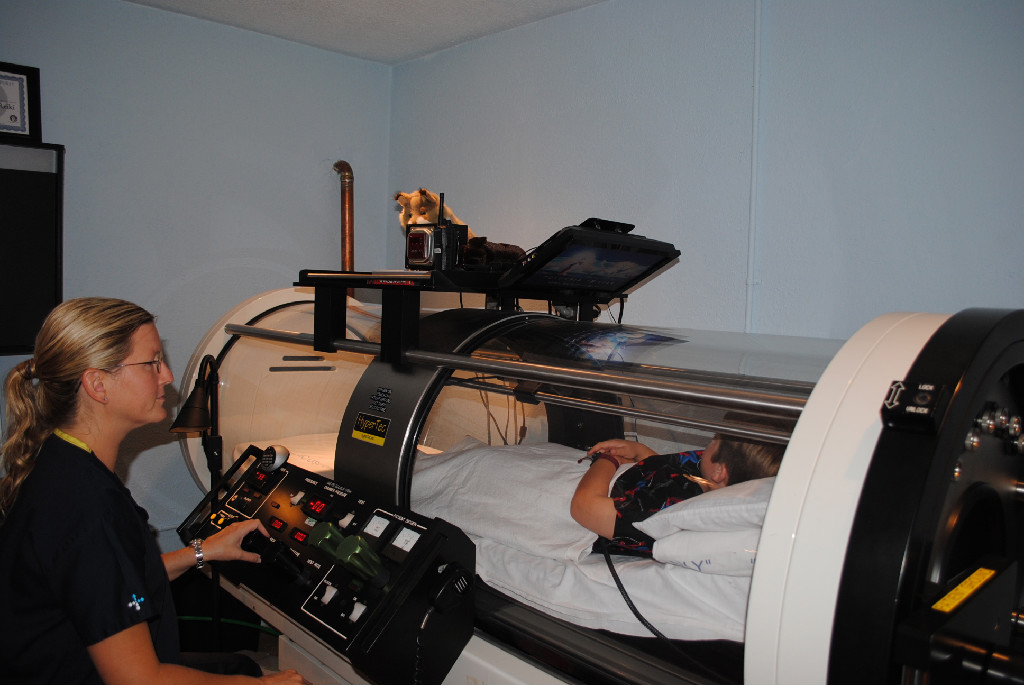
Hyperbaric oxygen therapy (HBOT) involves inhal- ing 100% oxygen at greater than one atmosphere absolute (ATA) in a pressurized chamber [9]. HBOT has been used successfully in humans at varying pressures to treat a range of conditions. Many clin- ical applications of HBOT are at higher pressures (over 2.0 ATA) including treatment of decompres- sion sickness, arterial gas embolism, carbon mon- oxide poisoning [10], amyotrophic lateral sclerosis [11], and complex regional pain syndrome [12]. However, HBOT has also been used at lower pres- sures (1.5 ATA or less) with clinical success in con- ditions including fetal alcohol syndrome [13] and ischemic brain injury [14]. HBOT at 1.5 ATA was utilized in a prospective trial of 168 patients with closed head trauma with a significant reduction in mortality (32% versus 17%) [15].
HBOT has been shown to increase the oxygen content of plasma [16] and body tissues [17] and can even normalize oxygen levels in ischemic tissue [18]. In fact, the amount of oxygen delivered by HBOT at 3.0 ATA and 100% oxygen is able to keep tissue viable even without oxygen input from circu- lating hemoglobin [17]. In rat models, HBOT has been shown to reduce the effects of hypoxia and ischemia on the neonatal brain [19]. Human studies demonstrate that HBOT causes mild vasoconstric- tion resulting in decreased blood flow [20,21] but at the same time causes increased oxygen delivery and levels in target tissues [16,17,20]. By causing mild vasoconstriction, HBOT can reduce edema in ischemic tissue [22] including the brain [20,23], which results in lowering intracranial pressure [20].
HBOT is generally considered safe [17] at oxygen pressures below 3.0 ATA and with treatment dura- tions of less than 120 min [10,13,24]. The use of HBOT in children appears generally safe, even at pressures of 2.0 ATA for 2 hours per day for up to 40 sessions [25]. The most common side effect of HBOT is middle ear barotrauma, which occurs in
approximately 2% of patients. The incidence of such barotrauma is decreased with pseudoephed- rine treatment before HBOT. Less common side ef- fects in descending order include sinus squeeze, serous otitis, claustrophobia, and reversible myo- pia. Seizures may occur infrequently in about 0.01–0.03% of patients [9].
Hypothesis
Multiple studies have revealed that autism is a neu- rodegenerative disease characterized by cerebral hypoperfusion, neuroinflammation, and increased oxidative stress. HBOT helps overcome hypoperfu- sion, has potent anti-inflammatory effects and re- duces oxidative stress. Furthermore, HBOT mobilizes stems cells from human bone marrow. Therefore, HBOT will improve symptoms of autism.
Improving cerebral hypoperfusion in autism
Evidence of decreased cerebral blood flow in autism and possible mechanisms of hypoperfusion
Even in the presence of normal magnetic resonance imaging (MRI) findings, focal areas of decreased cerebral blood flow occur in children with autism [26]. Multiple independent single photon emission computed tomography (SPECT) and positron emis- sion tomography (PET) research studies have dem- onstrated hypoperfusion to several areas of the autistic brain, most notably the temporal lobes [26–39]. Several studies show that reduced blood flow to the temporal regions and other brain areas correlates with many of the clinical findings associ- ated with autism including repetitive, self-stimula- tory and stereotypical behaviors, and impairments in communication, sensory perception, and social interaction [27,29,31,39–42]. Furthermore, a cor- relation between decreased IQ and hypoperfusion of the temporal and frontal lobes has been de- scribed in autistics [36].
The cause of this decreased blood flow is not known but may be secondary to changes in cerebral arterial resistance. Under normal conditions, cere- bral blood flow increases when local brain tissue metabolic rate and functioning increases [43,44]. However, this response may be reversed in autistic children. One of the first studies measuring cere- bral blood flow in autistic children utilized trans- cranial Doppler ultrasound and showed decreased
218
Rossignol and Rossignol
blood flow and concomitantly increased middle cerebral arterial resistance upon auditory stimula- tion. Conversely, control neurotypical and men- tally retarded children showed opposite results [45].
The mechanism of this abnormal change in cere- bral arterial resistance in autistic children is un- known. However, several studies have shown that astrocytes can regulate cerebral blood flow. Astro- cytes can directly cause arteriole vasoconstriction through a calcium mechanism [46] and arteriole vasodilatation through a cyclooxygenase medium [47]. Neurons, astrocytes, and vascular cells com- pose a functional unit that maintains proper blood flow and oxygenation for the brain [48]. Neural activity normally causes increased cerebral blood flow thus delivering increased oxygen [44]. How- ever, a recent study found evidence of neuroin- flammation and astroglial activation in autism [49]. It is possible that astroglial inflammation may affect the control of blood flow regulated by astrocytes and lead to the abnormal changes in cerebral artery resistance and hypoperfusion seen in some autistic children.
Furthermore, inflammation is a known cause of decreased blood flow and several inflammatory conditions have associated cerebral hypoperfusion including lupus [50,51], Sjo ̈gren’s syndrome [52], Behc ̧et’sdisease[53],viralencephalitis[54,55], and acute Kawasaki disease [40]. One SPECT study of 27 children with echovirus meningitis demon- strated decreased cerebral blood flow in 74% of the children [55] and two recent SPECT studies re- vealed impaired cerebral perfusion in 81% of pa- tients with Sjo ̈gren’s syndrome [52]. In one SPECT study of patients with systemic lupus erythemato- sus, 59% had evidence of cerebral hypoperfusion [51]. Furthermore, treatment of the inflammation found in lupus with iloprost [56] and methylpred- nisolone [57] normalized cerebral blood flow on follow-up SPECT scans. It is conceivable that the cerebral hypoperfusion found in autistic children may be triggered by neuroinflammation and there- fore may be reversible with anti-inflammatory modalities.
Zones of the autistic brain affected by decreased blood flow and symptom correlations
Cerebral hypoperfusion may play a role in some of the more unusual characteristics of autistic behav- ior. Diminished blood flow to the thalamus has been correlated with the autistic clinical features of repetitive, self-stimulatory, and unusual behav-
iors including resistance to changes in routine and environment [29]. Hypoperfusion of the temporal lobes has also been linked with increased autism symptom profile scores including ‘‘obsessive desire for sameness’’ and ‘‘impairments in communica- tion and social interaction’’ [31]. Another study on ‘‘high functioning’’ autistics demonstrated de- creased blood flow to areas of the temporal lobe and amygdala, which was correlated with clinical impairments in processing facial expressions and emotions [42]. This was confirmed by a recent study of autistics demonstrating diminished blood flow to the ‘‘fusiform face area’’ responsible for recognizing familiar faces [58].
In addition, decreased perfusion of the temporal lobes is a consistent finding in many studies of autistic children. Two larger controlled studies (21–23 autistic children) using SPECT and PET scans confirmed significant bitemporal hypoperfu- sion [31,34]. In both of these studies, the control group was mentally retarded; therefore, the hyp- operfusion could not be attributed to mental retar- dation alone [33,34]. Another SPECT study of 31 autistic children, 16 of whom had epilepsy, also demonstrated reduction of cerebral blood flow to the temporal lobes. Of note, cerebral blood flow was not different between those with and without epilepsy, suggesting that epilepsy itself was not associated with hypoperfusion in these individuals [37]. A more recent PET study of 11 autistic chil- dren revealed diminished blood flow to the left temporal area, including Wernicke’s area (which is involved in language comprehension) and Brod- mann’s area 21 (involved in auditory processing and language), when compared to age-matched mentally retarded children [39]. Interestingly, an association between temporal lobe abnormalities [59] and the subsequent development of secondary autism has been described in tuberous sclerosis [60], infantile spasms [61], herpes simplex enceph- alitis [62,63], and an acute encephalopathic illness in children [64].
The relative amount of cerebral hypoperfusion in autistic children can vary by age. In one study, hypoperfusion of the prefrontal and left temporal areas worsened and became ‘‘quite profound’’ as the age of the autistic child increased. This dimin- ished perfusion correlated with decreased lan- guage development. The authors concluded that hypoperfusion ‘‘subsequently prevents develop- ment of true verbal fluency and development in the temporal and frontal areas associated with speech and communication’’ [27].
Hypoperfusion of the temporal and other brain regions has been correlated with many of the clin- ical findings associated with autism including self-
Hyperbaric oxygen therapy may improve symptoms in autistic children 219
stimulatory behaviors and impairments in commu- nication, sensory perception, and social interaction [33,34]. This diminished blood flow may be medi- ated by neuroinflammation. Further studies on the effects of inflammation on blood flow in the autistic brain are needed, especially studies involv- ing the temporal lobes where hypoperfusion is common. Whatever the cause of the hypoperfu- sion, the possibility exists that the enhancement of oxygen delivery to the brain accomplished by HBOT may improve some of the symptoms found in autistic children.
The use of HBOT in cerebral hypoperfusion disorders
The oxygen delivered by HBOT can reverse hypoxia in brain tissues caused by hypoperfusion [65,66]. Cerebral hypoperfusion causes hypoxia, which trig- gers electrical failure in brain cells. Worsening hy- poxia then eventually results in ion pump failure, which ultimately leads to cell death [67]. Cells that have electrical failure but retain ion pump ability have been described as ‘‘idling’’ because they re- main alive but non-functional [68]. SPECT studies have confirmed the presence of these ‘‘idling cells,’’ which surround areas of focal ischemia and comprise what is termed the ‘‘ischemic pen- umbra’’ [69]. Restoration of oxygenation, some- times even years after the ischemic insult, can salvage these cells, which may explain why the acute findings of a stroke are poor predictors of ultimate clinical outcomes [67].
Even though HBOT causes decreased cerebral blood flow through vasoconstriction [70], it simul- taneously causes increased cerebral oxygen tension [20] and may accelerate brain recovery from ische- mia [71]. In one case report, 80 sessions of HBOT at 1.5 ATA increased oxygenation to the ischemic penumbra on SPECT scans and significantly im- proved cognitive and motor function in a patient with an ischemic brain injury from a near drowning episode 12 years earlier [14]. Another study of three patients with brain injuries showed areas of ‘‘dormant’’ neurons in the ischemic penumbra on SPECT scans prior to the commencement of HBOT at 1.5 ATA. All three patients had improvement in the oxygenation of these areas as seen on post- HBOT SPECT scans, which was correlated with clin- ical improvement [65].
HBOT has been used with clinical effectiveness in some cerebral hypoperfusion disorders includ- ing lupus [72] and traumatic midbrain syndrome [73], and may be beneficial in acute ischemic stroke [74] and acute myocardial infarction [16].
In addition, HBOT has been used in several stud- ies on children with cerebral palsy (CP). Some children with CP due to perinatal asphyxia have focal areas of cerebral hypoperfusion on SPECT scans [75]. Significant clinical improvements were found in one study of children with CP after 20 sessions of HBOT at 95% oxygen and 1.75 ATA [76].
Other studies using HBOT in cerebral hypoperfu- sion disorders have been performed at lower pres- sures (1.5 ATA or less). Stoller recently reported on one pediatric case of fetal alcohol syndrome, which is considered ‘‘irreversible and incurable’’ [13] and is characterized by cerebral hypoperfusion on SPECT studies [77]. Using HBOT at 1.5 ATA, the child had statistically significant improvements in verbal, memory, reaction time, impulse control, and visual motor scores [13]. In addition, Heuser et al. [78] treated a four year old autistic child using lower pressure HBOT at 1.3 ATA and reported ‘‘striking improvement in behavior including mem- ory and cognitive functions’’ after only ten ses- sions. Furthermore, the child had improvement of cerebral hypoperfusion as measured by pre-HBOT and post-HBOT SPECT scans [78]. These case re- ports are notable because they demonstrate that some ‘‘irreversible’’ and permanent neurological conditions can have clinical improvements with HBOT.
The number of HBOT sessions needed to produce full clinical improvements from cerebral hypoper- fusion or ischemia is unclear. In one study combin- ing the use of SPECT and HBOT, an average of 70 treatments was needed to show a significant in- crease in cerebral blood oxygenation and metabo- lism in patients with chronic neurological disorders including CP, stroke, and traumatic brain injury. Of note, the rate of improvement in cere- bral blood oxygenation was more profound during the last 35 treatments compared to the first 35 [79]. In addition, reports from some HBOT researchers indicate that younger patients tend to have improvements more quickly than older pa- tients [79]. Therefore, older patients may need more treatments.
Since many autistic children experience at least a mild degree of cerebral hypoperfusion, this de- creased blood flow could lead to an element of brain hypoxia. Multiple SPECT studies have shown evidence of relative brain hypoxia in certain cere- bral hypoperfusion syndromes, including autism [78], which improved after HBOT [14,65,78,79]. It is certainly plausible that the increased oxygen delivery by HBOT could overcome any hypoxia caused by hypoperfusion and thus lead to improve- ments in the symptoms of autistic children.
220
Rossignol and Rossignol
Improving neuroinflammation in autism
Evidence of neuroinflammation in autism
Recent studies reveal that autism is characterized by neuroinflammation. Autopsy brain samples of autistic patients demonstrate an active neuroin- flammatory process in the middle frontal gryus, anterior cingulate gryus, and cerebellar hemi- spheres including increased microglial and astrog- lial activation and increased proinflammatory cytokines. Furthermore, cerebrospinal fluid ob- tained from living autistic patients also ‘‘showed a prominent proinflammatory profile’’ [49]. Previous studies of autistic children have shown circulating serum autoantibodies to brain elements including neuron-axon filament protein and glial fibrillary acidic protein [80], the caudate nucleus, cerebral cortex and cerebellum [81,82] and neuron-specific antigens including myelin basic protein [83,84].
Inflammation in autistic children is not limited to the brain. When compared to typical children, autistic children make significantly more serum antibodies against gliadin and casein peptides [85], produce more pro-inflammatory cytokines [86], and have an imbalance of CD4+ and CD8+ cells [87]. Furthermore, some patients with autism have mucosal inflammation of the stomach, small intes- tine and colon characterized by ileo-colonic lym- phoid nodular hyperplasia [88]. In these children, the gastrointestinal mucosa has evidence of proin- flammatory cytokines [89], increased lymphocytic density, and epithelial IgG deposits mimicking an autoimmune lesion [90].
Several different therapies have been employed in treating the inflammation found in autistic chil- dren with some clinical success, including intrave- nous immune globulin [91]. Further research is needed to clarify the role of inflammation in aut- ism and to investigate potential therapies [92]. However, HBOT may be useful in decreasing inflam- mation found in autistic patients and may thereby improve symptoms.
HBOT use in inflammatory conditions
Several animal studies have revealed that HBOT has potent anti-inflammatory tissue effects [93,94] with equivalence to diclofenac 20 mg/kg noted in one study using HBOT at 2.4 ATA and 100% oxygen [95]. HBOT has also been shown to decrease the symptoms of advanced arthritis in rats [96] and attenuates the inflammatory response in the perito- neal cavity caused by injected meconium [97]. In addition, one animal study using HBOT at 2.5 ATA
showed increased survival and decreased protein- uria, anti-dsDNA antibody titers, and immune-com- plex deposition in lupus-prone autoimmune mice [98]. Furthermore, HBOT has been used in animal studies to improve colitis [93]. Interestingly, thirty sessions of HBOT at 2.0 ATA has been used in hu- mans to achieve remission of ulcerative colitis not responding to conventional therapies [99]. This may be relevant in autistic children given the higher prevalence of gastrointestinal mucosal inflamma- tion described previously. Given the results of these studies, it is certainly plausible that HBOT can de- crease both neuroinflammation and gastrointestinal inflammation in autistic children and thereby potentially lead to improvements in symptoms.
Improving oxidative stress in autism
Evidence of increased oxidative stress in autism
Recent studies have shown that autistic children have evidence of increased oxidative stress includ- ing lower serum glutathione levels [100]. Sogut et al. [101] demonstrated that autistic children had increased red blood cell nitric oxide, which is a known reactive free radical and is toxic to the brain [101]. James et al. [100] recently showed that total serum glutathione levels were 46% lower and oxidized glutathione was 72% higher in autistic children when compared to neurotypical controls. This was reflected in a lower redox ratio of reduced glutathione to oxidized glutathione, which presum- ably led to decreased antioxidant ability in these autistic children [100]. Lower serum antioxidant enzyme, antioxidant nutrient, and glutathione lev- els, as well as higher pro-oxidants have been found in multiple studies of autistic children [102]. Fur- thermore, treatment with anti-oxidants has been shown to raise the levels of reduced glutathione in the serum of autistic children and appears to im- prove symptoms [100]. It is speculated that treat- ment with hyperbaric oxygen may also help reduce oxidative stress in autistic children.
The effect of HBOT on oxidative stress
Multiple studies have shown neutral effects on oxi- dative stress with HBOT use [103]. In one study on horse platelets, measures of oxidative stress were not increased after HBOT; in fact, a rise in the anti- oxidant enzyme superoxide dismutase (SOD) was found 24 h after HBOT without a fall in glutathione levels [104]. In another study on dogs, following 18 min of complete cerebral ischemia, HBOT at
Hyperbaric oxygen therapy may improve symptoms in autistic children 221
2.0 ATA reduced brain damage without increasing oxidative stress [105]. Furthermore, in a rat model of reperfusion, HBOT extended skin flap life with- out evidence of oxidative stress [106].
In addition, numerous studies have shown improvements in oxidative stress with HBOT includ- ing increased production of antioxidants and antiox- idant enzymes and decreased markers of oxidative stress such as malondialdehyde [105,107,108]. An improvement in the survival rate of skin flaps and an increase in SOD levels were found in one study when rats were exposed to hyperbaric oxygen at 2.0 ATA [109]. In another study, HBOT at 2.5 ATA in- duced the production of antioxidants and decreased malondialdehyde levels in rats [107]. Furthermore, in a study of rats with pancreatitis, HBOT at 2.5 ATA decreased oxidative stress markers including malondialdehyde, and increased the levels of the anti-oxidant enzymes glutathione peroxidase and SOD [108]. HBOT has also been shown to acutely raise the levels of reduced glutathione in the plasma and lymphocytes of some humans after just one treatment session at 2.5 ATA [110]. Finally, ische- mia-reperfusion injuries usually cause oxidative stress through decreases in glutathione levels and activities of catalase and SOD. However, in one rat study of ischemia, pretreatment with 1–3 doses of HBOT caused an increase in liver glutathione and SOD levels and protected against liver injury; con- trol animals not receiving HBOT actually had drops in glutathione and anti-oxidant enzyme levels and had concomitant liver damage [111].
HBOT, reactive oxygen species, and anti-oxidants
Concerns have been raised that HBOT may cause in- creased oxidative stress through the production of reactive oxygen species [112]. This concern is con- troversial as studies have shown mixed results. Contrary to the studies discussed previously, sev- eral studies using HBOT at 2.5 ATA or greater have found evidence of increased oxidative stress [113– 115]. Support for this higher pressure effect was found in one study, which demonstrated that HBOT at 2.0 ATA increased SOD levels whereas HBOT at 3.0 ATA caused SOD levels to decrease, presumably because the SOD had to neutralize more free radi- cals at the 3.0 ATA pressure [116]. Thus, from an oxidative stress and SOD production standpoint, there might be an optimal HBOT pressure, which falls somewhere below 2.5 ATA.
Along a similar line of thought, some authors have speculated that a limited quantity of reactive oxygen metabolites may actually have beneficial
effects in the human body [117–119]. The produc- tion of small amounts of oxygen radicals may con- fer protection from future hypoxia and this effect has been termed ‘‘ischemic tolerance.’’ In one ani- mal study, pre-treatment with HBOT at 2.0 ATA prior to an ischemia insult induced ischemic toler- ance whereas pre-treatment at 3.0 ATA did not, possibly because this higher pressure may have generated too many oxygen radicals [116].
Nevertheless, many studies demonstrate that HBOT lowers oxidative stress. Furthermore, oxida- tive stress appears to be less of a concern at pres- sures under 2.0 ATA, which are often used clinically [116]. In spite of this, therapies to raise glutathi- one levels [100] and the use of antioxidants [120] may be beneficial in patients with conditions of in- creased oxidative stress before HBOT is contem- plated. Several antioxidant supplements have been found to attenuate oxidative stress induced by high pressure HBOT including a-lipoic acid [112], melatonin [121], N-acetylcysteine [111,122], vitamin E [123], riboflavin [124], sele- nium [123,124], and glutathione [125]. Based upon these findings, a combination of antioxidants and HBOT may help reduce oxidative stress in autistic children and lead to improvements in symptoms.
Improving stem cell mobilization in autism
Recently, HBOT at 2.0 ATA and 100% oxygen for 2 h was shown to mobilize stem/progenitor cells from the bone marrow of humans. Elevations were found in the number of colony-forming cells as demon- strated by an increase in the number of CD34+ cells by almost 2-fold [126]. This finding is relevant be- cause autism and hypoxic brain injuries are consid- ered by many to be permanent conditions. However, new research is revealing that even long-standing brain disorders may be partially reversible [13,14]. Recently, stem cells have been isolated in the adult brain. This leads to the possi- bility of neuropoiesis, or regrowth, of certain brain cells. A possible scenario for inducing brain repair through the use of existing mature brain stem cells has been described and is dependent on an intact vascular supply and adequate oxygen [127], both of which can be enhanced by HBOT.
Testing the hypothesis
There is a strong possibility that HBOT could play an integral role in improving brain disorders associ- ated with hypoxia, hypoperfusion, inflammation,
222
Rossignol and Rossignol
Table 1 Summary of HBOT use in autism
Autism
. Cerebral perfusion m Inflammation m Oxidative stress Neurodegenerative
disease
HBOT
m Perfusion to brain tissue . Inflammation . Oxidative stress m Stem cells
and/or oxidative stress, including autism, through the improvement of oxygen supply, decreased inflammation and oxidative stress, and/or the recruitment of new stem cells (see Table 1). This in turn should lead to improved clinical outcomes. Some physicians have begun using HBOT in autistic children and anecdotal reports indicate that HBOT has improved symptoms in autistic children includ- ing enhancements in socialization, language, and repetitive behaviors [78,128]. A recent retrospec- tive case series also indicates that low pressure HBOT may improve symptoms in autistic children (see Appendix A). Further research in this area, including HBOT trials in autistic patients, is ur- gently needed to test this hypothesis.
Acknowledgments
The authors thank the following for reviewing this manuscript and offering advice: Dr. John Battiston, Dr. Bentley Calhoun, Mr. Michael Haynes, Dr. Eliza- beth Mumper, Dr. David Slawson, and Dr. Kyle Van Dyke. Written consent was obtained from the chil- dren’s parent(s) for publication of case series data. The authors have two autistic sons who partici- pated in the case series.
Appendix A. Low pressure hyperbaric oxygen therapy1 improves symptoms in autistic children: A retrospective case series
Background
Since low pressure HBOT (under 1.5 ATA) improved symptoms in some patients with cerebral hypoper-
1 Hyperbaric oxygen therapy (HBOT) normally refers to inhal- ing 100% oxygen at greater than 1 ATA in a pressurized chamber [9]. However, for the purposes of this case series, the treatment with hyperbaric pressure at 1.3 ATA augmented with 28–30% oxygen is referred to as HBOT. Hyperbaric pressure at 1.3 ATA and room air is simply termed hyperbaric therapy.
fusion disorders [13–15,65], it was hypothesized that low pressure HBOT would also help autism, a disease in which cerebral hypoperfusion is an inte- gral component [31,32]. Recently, evidence has accumulated that low pressure hyperbaric therapy at 1.3 ATA and less than 100% delivered oxygen may improve symptoms in some diseases associated with cerebral hypoperfusion. For instance, one study using hyperbaric therapy at 1.3 ATA and room air demonstrated clinical improvements in some children with CP [129,130], a disease shown to have evidence of diminished cerebral blood flow [75]. Furthermore, one case report indicated ‘‘striking improvement’’ in a 4 year old child with autism after using hyperbaric therapy for 10 ses- sions at 1.3 ATA and room air. The child also had improvement of cerebral hypoperfusion as mea- sured by pre-HBOT and post-HBOT SPECT scans [78]. Based upon these findings, it was hypothe- sized that low pressure HBOT would improve symp- toms of autism. A retrospective case series was examined to evaluate this hypothesis. A review of the medical literature was performed using MED- LINE and Google Scholar and no clinical studies were found on the use of HBOT in autistic children.
Methods
This study is a retrospective analysis of 6 autistic children who underwent low-pressure HBOT. All 6 children had a prior diagnosis of autism (DSM-IV 299.00) by an outside physician and none of the children had previously received HBOT. In the nor- mal course of treatment, parent-rated scales were obtained pre-treatment and post-treatment. The University of Virginia Institutional Review Board for Health Sciences Research approved our retro- spective examination of cases in this study and for the use of this data for publication.
Informed consent was obtained from each child’s parent(s) prior to starting HBOT. All 6 chil- dren started and 5 completed 40 1 h sessions of low pressure HBOT at 1.3 ATA and 28–30% oxygen (after adjustment for the pressure effect) over a three month period. One child (Child C) only fin- ished twenty-five sessions due to scheduling con- flicts and was included in the analysis. All 6 children were taking multiple antioxidant supple- ments before starting HBOT. Children were allowed to continue all current therapies and to add new ones during HBOT. The characteristics of the chil- dren, including age and sex, are found in Table 2.
A low pressure hyperbaric chamber was used. Room air mixed with oxygen from an oxygen concentrator was pumped into the pressurized
Hyperbaric oxygen therapy may improve symptoms in autistic children 223
Table 2 Patient characteristics and scoresa
Child Age
A 2 B 4 Cb 3 D 7
Sex ATEC before HBOT
M 40 M 91 M 75 M 35
ATEC after HBOT
22 55 64 32 80 22
CARS before HBOT
21 37.5 45 27 41.5 23
CARS after HBOT
SRS before HBOT
17 30 38 25 39.5 22 54
SRS after HBOT
44 110 121 62 121 67
E F
6 F 7 F
88 24
98 154 135 94 139
a Declining scores indicate improvement on these scales. b Received only 25 HBOT treatments.
Table 3 Average score changesa by age
Age
4 and under 5 and older All children
ATEC before HBOT
68.7 49.0 58.8
ATEC after CARS before HBOT HBOT
47.0 34.5 44.7 30.5 45.8 32.5
CARS after HBOT
28.3 28.8 28.6
SRS before HBOT
129.0 95.7 112.3
SRS after HBOT
91.7 83.3 87.5
a Declining scores indicate improvement on these scales.
chamber, resulting in a final chamber oxygen con- centration of 28–30% by direct oximetry measure- ment using a Moxyä oxygen monitor and after adjustment for the pressure effect. Multiple ran- dom oximetry measurements were taken on differ- ent treatment days to verify the consistency of the chamber oxygen concentration, which uniformly remained 28–30%. Parent rated pre-treatment scores and post-treatment scores were calculated for each subject (see Table 2) using the Autism Treatment Evaluation Checklist (ATEC), Childhood Autism Rating Scale (CARS), and Social Responsive- ness Scale (SRS). ATEC is a scoring system of verbal communication, sociability, sensory/cognitive awareness, and health/autistic behaviors published by the Autism Research Institute [131]. CARS is a widely used scale for screening and diagnosing aut- ism and has been shown to correlate very well with
the DSM-IV criteria for autism diagnosis [132]. SRS is a recently validated test of interpersonal behav- ior, communication, and stereotypical traits in autism [133].
Results
Low pressure HBOT was well tolerated by all 6 chil- dren with no adverse effects noted. More dramatic improvements were found in children age 4 and under when compared to those in the older group (Table 3).
ATEC score results
The average improvement in all children on ATEC was 22.1% (p = 0.0538) ( Fig. 1). ATEC scores im- proved by 31.6% in the younger group compared to 8.8% in the older group (Fig. 2).
100 80 60 40 20 0
Before HBOT
After 40 HBOT
Figure 1 ATEC scores for all children.
Child A Child C Child E Child B Child D Child F
80 60 40 20
0
Before HBOT
After 40 HBOT
Figure 2 ATEC scores by age.
Age Under 5 Age Over 5
Score
Score
224
Rossignol and Rossignol
CARS score results
The average improvement in all children on CARS was 12.1% (p=0.0178) (Fig. 3). CARS improved
18.0% in the younger group and 5.6% in the older group (Fig. 4).
SRS score results
The average improvement in all children on SRS was 22.1% (p = 0.0518) (Fig. 5). SRS improved 28.9% in the younger group and 13.0% in the older group (Fig. 6).
Discussion
Autism is characterized, in part, by decreased cerebral blood flow [31,32]. Low pressure HBOT has been used in some cerebral hypoperfusion conditions including CP. Recently, a study demon- strated that some children with CP had clinical improvements using hyperbaric therapy at 1.3 ATA. In this study, 111 patients with CP and a his- tory of hypoxia in the perinatal period had statis- tically significant clinical improvements in gross motor function, memory, attention, and language production after hyperbaric therapy. One group received lower pressure hyperbaric therapy at 1.3 ATA and room air while the other group was given higher pressure HBOT at 1.75 ATA and 100% oxygen. Interestingly, the improvements in symptoms were statistically equivalent in the two groups [129]. Most of the improvements con- tinued for 3 months after treatment and some of the children from the study began walking, speak- ing, and sitting for the first times in their lives [130]. However, it must be noted that this study was controversial, as children in the lower pres- sure group improved equally with children in the higher pressure group. However, based on these findings, it was hypothesized that low-pressure HBOT could potentially improve symptoms in autistic children.
This case series suggests that low pressure HBOT may indeed be beneficial in the treatment of aut- ism. An interesting finding from this case series was that the younger children had more significant improvements in clinical outcome scores than the older children. This is congruent with reports from some HBOT researchers indicating that younger pa- tients tend to have improvements more quickly than older patients [79]. This effect may be par- tially explained by the findings of a previous study, which showed that autistic children aged 3–4 years experience diminished frontal lobe blood flow com- pared to age-matched neurotypical children [41]. It is possible that HBOT in younger autistic children can improve cerebral oxygenation and thus over- come the effects of hypoperfusion and aid these children in ‘‘catching up’’ with their neurotypical
50 40 30 20 10
0
Before HBOT
After 40 HBOT
Figure 3 CARS scores for all children.
Child A Child C Child E Child B Child D Child F
40 30 20 10
0
Before HBOT
After 40 HBOT
Figure 4 CARS scores by age.
Age Under 5 Age Over 5
180 160 140 120 100
80 60 40 20
0
Before HBOT
After 40 HBOT
Figure 5 SRS scores for all children.
Child A Child C Child E Child B Child D Child F
140 120 100
80 60 40 20
0
Before HBOT
After 40 HBOT
Figure 6 SRS scores by age.
Age Under 5
Age Over 5
Score Score Score Score
Hyperbaric oxygen therapy may improve symptoms in autistic children 225
peers. Furthermore, the younger children in this case series may have had less overall hypoperfusion to surmount because decreased cerebral blood flow to areas associated with communication has been shown to worsen with increasing age in autistic children [27]. It is likely that the older children in this case series need more than 40 HBOT sessions to show further improvements, especially since some HBOT researchers have noted that 50–80 HBOT sessions are typically needed to show signif- icant clinical gains [79]. In addition, the chamber was augmented with only 28–30% oxygen instead of 100% oxygen. It is possible that the children in this case series may have experienced more improvements if 100% oxygen and/or a higher pres- sure had been used. These speculations certainly warrant further testing.
This case series did have several inherent limi- tations. Children were allowed to continue all other therapies for autism and also add new ones, such as supplements. Therefore, other therapies could have contributed to the some of the clinical gains. Parents were not blinded to the fact that their children received HBOT and evaluation of the children was through parent-rated scales, either of which could lead to bias. There was no placebo or control group. Thus, the improvements could have been due merely to the natural development of the children, although none of the parents reported their child as undergoing developmental spurts of similar or greater magni- tude in the recent past. Finally, this series lacked power because the sample size was small. Despite these limitations, the analysis of this case series suggests substantial clinical benefits were pro- duced, and therefore, this hypothesis needs to be tested in a formal prospective study.
Conclusions
HBOT has been shown to increase oxygen delivery to hypoperfused or hypoxic tissues, decrease inflammation and oxidative stress, and mobilize stem cells from human bone marrow. The mecha- nism of clinical improvements in ATEC, CARS, and SRS scores in the children studied may be second- ary to increased oxygenation of underperfused areas of the autistic brain, reduced neuroinflam- mation, decreased oxidative stress, or a combina- tion of these. This case series suggests that low pressure HBOT improves symptoms in autistic chil- dren. Further research in this area, including HBOT trials in autistic patients, using observers blinded to the intervention, is now needed to test this hypothesis.
References
[1] Singh N (contact). Press release: CDC launches ‘‘Learn the signs. Act early.’’ Campaign, http://www.cdc.gov/od/ oc/media/pressrel/r050222.htm; February 22, 2005 [accessed 21.01.06].
[2] Kanner L. Autistic disturbances of affective contact. Nervous Child 1943;2:217–50.
[3] Rapin I. Autism. N Engl J Med 1997;337(2):97–104. [4] Wing L, Potter D. The epidemiology of autistic spectrum disorders: is the prevalence rising? Ment Retard Dev Disabil
Res Rev 2002;8(3):151–61. [5] Stokstad E. New hints into the biological basis of autism.
Science 2001;294:34–7. [6] Muhle R, Trentacoste SV, Rapin I. The genetics of autism.
Pediatrics 2004;113:472–86. [7] Centers for Disease Control and Prevention. How common
is autism spectrum disorder? www.cdc.gov/ncbddd/aut- ism/asd_common.htm; February 17, 2005 [accessed 21.01.06].
[8] Gillberg C, Wing L. Autism: not an extremely rare disorder. Acta Psychiatr Scand 1999;99(6):399–406.
[9] Feldmeier JJ. Chairman and Editor. Hyperbaric oxygen 2003: indications and results: the hyperbaric oxygen therapy committee report. Kensington, MD: Undersea and Hyperbaric Medical Society; 2003.
[10] Leach RM, Rees PJ, Wilmshurst P. ABC of oxygen: hyperbaric oxygen therapy. BMJ 1998;317:1140–3.
[11] Steele J, Matos LA, Lopez EA, et al. A phase 1 safety study of hyperbaric oxygen therapy for amyotrophic lateral sclerosis. ALS 2004;5:250–4.
[12] Kiralp MZ, Yildiz S, Vural D, Keskin I, Ay H, Dursun H. Effectiveness of hyperbaric oxygen therapy in the treat- ment of complex regional pain syndrome. J Int Med Res 2004;32:258–62.
[13] Stoller KP. Quantification of neurocognitive changes before, during, and after hyperbaric oxygen therapy in a case of fetal alcohol syndrome. Pediatrics 2005;116:586–91.
[14] Neubauer RA, Gottlieb SF, Miale A. Identification of hypometabolic areas in the brain using brain imaging and hyperbaric oxygen. Clin Nucl Med 1992;17(6):477–81.
[15] Rockswold GL, Ford SE, Anderson DC, Bergman TA, Sherman RE. Results of a prospective randomized trial for the treatment of severely brain-injured patients with hyperbaric oxygen. J Neurosurg 1992;76(6):929–34.
[16] Shandling AH, Ellestad MH, Hart GB, et al. Hyperbaric oxygen and thrombolysis in myocardial infarction: the ‘‘HOT MI’’ pilot study. Am Heart J 1997;134:544–50.
[17] Gill AL, Bell CAN. Hyperbaric oxygen: its uses, mechanisms of action and outcomes. Q J Med 2004;97:385–95.
[18] Ackerman NB, Brinkley FB. Oxygen tensions in normal and ischemic tissues during hyperbaric therapy. JAMA 1966;198(12):1280–3.
[19] Calvert JW, Yin W, Patel M, et al. Hyperbaric oxygenation prevented brain injury induced by hypoxia-ischemia in a neonatal rat model. Brain Res 2002;951:1–8.
[20] Sukoff MH, Ragatz RE. Hyperbaric oxygenation for the treatment of acute cerebral edema. Neurosurgery 1982;10(1):29–38.
[21] Bird AD, Telfer AB. Effect of hyperbaric oxygen on limb circulation. Lancet 1965;13:355–6.
[22] Nylander G, Lewis D, Nordstrom H, Larsson J. Reduction of postischemic edema with hyperbaric oxygen. Plast Rec- onstr Surg 1985;76(4):596–603.
[23] Veltkamp R, Siebing DA, Sun L, et al. Hyperbaric oxygen reduces blood-brain barrier damage and edema after
226
Rossignol and Rossignol
transient focal cerebral ischemia. Stroke 2005;36:
1679–83. [24] Nuthall G, Seear M, Lepawsky M, Wensley D, Skippen P,
Hukin J. Hyperbaric oxygen therapy for cerebral palsy: two complications of treatment. Pediatrics 2000;106(6): E80.
[25] Ashamalla HL, Thom SR, Goldwein JW. Hyperbaric oxygen therapy for the treatment of radiation-induced sequelae in children: the University of Pennsylvania experience. Cancer 1996;77(11):2407–12.
[26] Ryu YH, Lee JD, Yoon PH, Kim DI, Lee HB, Shin YJ. Perfusion impairments in infantile autism on techne- tium-99m ethyl cysteinate dimer brain single-photon emission tomography: comparison with findings on mag- netic resonance imaging. Eur J Nucl Med 1999;26(3): 253–9.
[27] Wilcox J, Tsuang MT, Ledger E, Algeo J, Schnurr T. Brain perfusion in autism varies with age. Neuropsychobiology 2002;46:13–6.
[28] Chiron C, Leboyer M, Leon F, Jambaque I, Nuttin C, Syrota A. SPECT of the brain in childhood autism: evidence for a lack of normal hemispheric asymmetry. Dev Med Child Neurol 1995;37(10):849–60.
[29] Starkstein SE, Vazquez S, Vrancic D, et al. SPECT findings in mentally retarded autistic individuals. J Neuropsychia- try Clin Neurosci 2000;12:370–5.
[30] Mountz JM, Tolbert LC, Lill DW, Katholi CR, Liu HG. Functional deficits in autistic disorder: characterization by technetium-99m-HMPAO and SPECT. J Nucl Med 1995;36(7):1156–62.
[31] Ohnishi T, Matsuda H, Hashimoto T, et al. Abnormal regional cerebral blood flow in childhood autism. Brain 2000;123:1838–44.
[32] George MS, Costa DC, Kouris K, Ring HA, Ell PJ. Cerebral blood flow abnormalities in adults with infantile autism. J Nerv Ment Dis 1992;180(7):413–7.
[33] Boddaert N, Zilbovicius M. Functional neuroimaging and childhood autism. Pediatr Radiol 2002;32:1–7.
[34] Zilbovicius M, Boddaert N, Belin P, et al. Temporal lobe dysfunction in childhood autism: a PET study. Am J Psychiatry 2000;157:1988–93.
[35] Kaya M, Karasalihoglu S, Ustun F, et al. The relationship between 99mTc-HMPAO brain SPECT and the scores of real life rating scale in autistic children. Brain Dev 2002;24:77–81.
[36] Hashimoto T, Sasaki M, Fukumizu M, Hanaoka S, Sugai K, Matsuda H. Single-photon emission computed tomography of the brain in autism: effect of the developmental level. Pediatr Neurol 2000;23:416–20.
[37] Gillberg IC, Bjure J, Uvebrant P, Vestergren E, Gillberg C. SPECT (single photon emission computed tomography) in 31 children and adolescents with autism and autism- like conditions. Eur Child Adolesc Psychiatry 1993;2(1): 50–9.
[38] Boddaert N, Belin P, Chabane N, et al. Perception of complex sounds: abnormal pattern of cortical activation in autism. Am J Psychiatry 2003;160:2057–60.
[39] Boddaert N, Chabane N, Belin P, et al. Perception of complex sounds in autism: abnormal auditory cortical processing in children. Am J Psychiatry 2004;161: 2117–20.
[40] Ichiyama T, Nishikawa M, Hayashi T, Koga M, Tashiro N, Furukawa S. Cerebral hypoperfusion during acute Kawa- saki disease. Stroke 1998;29:1320–1.
[41] Zilbovicius M, Garreau B, Samson Y, et al. Delayed maturation of the frontal cortex in childhood autism. Am J Psychiatry 1995;152(2):248–52.
[42] Critchley HD, Daly EM, Bullmore ET, et al. The functional neuroanatomy of social behaviour: changes in cerebral blood flow when people with autistic disorder process facial expressions. Brain 2000;123:2203–12.
[43] Fox PT, Raichle ME. Focal physiological uncoupling of cerebral blood flow and oxidative metabolism during somatosensory stimulation in human subjects. Proc Natl Acad Sci USA 1986;83:1140–4.
[44] Parri R, Crunelli V. An astrocyte bridge from synapse to blood flow. Nat Neurosci 2003;6(1):5–6.
[45] Bruneau N, Dourneau MC, Garreau B, Pourcelot L, Lelord G. Blood flow response to auditory stimulations in normal, mentally retarded, and autistic children: a preliminary transcranial Doppler ultrasonographic study of the middle cerebral arteries. Biol Psychiatry 1992;32:691–9.
[46] Mulligan SJ, MacVicar BA. Calcium transients in astrocyte endfeet cause cerebrovascular constrictions. Nature 2004;431:195–9.
[47] Zonta M, Angulo MC, Gobbo S, et al. Neuron-to-astrocyte signaling is central to the dynamic control of brain microcirculation. Nat Neurosci 2003;6(1):43–50.
[48] Iadecola C. Neurovascular regulation in the normal brain and in Alzheimer’s disease. Nat Rev Neurosci 2004;5: 347–60.
[49] Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA. Neuroglial activation and neuroinflammation in the brain of patients with autism. Ann Neurol 2005;57:67–81.
[50] Huang WS, Chiu PY, Tsai CH, Kao A, Lee CC. Objective evidence of abnormal regional cerebral blood flow in patients with systemic lupus erythematosus on Tc-99m ECD brain SPECT. Rheumatol Int 2002;22:178–81.
[51] Postiglione A, De Chiara S, Soricelli A, et al. Alterations of cerebral blood flow and antiphospholipid antibodies in patients with systemic lupus erythematosus. Int J Clin Lab Res 1998;28:34–8.
[52] Lass P, Krajka-Lauer J, Homziuk M, et al. Cerebral blood flowinSjo ̈gren’ssyndromeusing99Tcm-HMPAObrain SPET. Nucl Med Commun 2001;21:31–5.
[53] Caca I, Nazaroglu H, Unlu K, Cakmak SS, Ari S, Sakalar YB. Color Doppler imaging of ocular hemodynamic changes in Beh ̧cet’s disease. Jpn J Ophthalmol 2004;48:101–5.
[54] Wakamoto H, Ohta M, Nakano N, Kunisue K. SPECT in focal enterovirus encephalitis: evidence for local cerebral vasculitis. Pediatr Neurol 2000;23:429–31.
[55] Nishikawa M, Matsubara T, Yoshitomi T, Ichiyama T, Hayashi T, Furukawa S. Abnormalities of brain perfusion in echovirus type 30 meningitis. J Neurol Sci 2000;179: 122–6.
[56] Mathieu A, Sanna G, Mameli A, et al. Sustained normal- ization of cerebral blood-flow after iloprost therapy in a patient with neuropsychiatric systemic lupus erythemat- osus. Lupus 2002;11:52–6.
[57] Liu FY, Huang WS, Kao CH, Yen RF, Wang JJ, Ho ST. Usefulness of Tc-99m ECD brain SPECT to evaluate the effects of methylprednisolone pulse therapy in lupus erythematosus with brain involvement: a preliminary report. Rheumatol Int 2003;23:182–5.
[58] Pierce K, Haist F, Sedaghat F, Courchesne E. The brain response to personally familiar faces in autism: findings of fusiform activity and beyond. Brain 2004;127:2703–16.
[59] Bachevalier J. Medial temporal lobe structures and autism: a review of clinical and experimental findings. Neuropsychologia 1994;32(6):627–48.
[60] Bolton PF, Griffiths PD. Association of tuberous sclerosis of temporal lobes with autism and atypical autism. Lancet 1997;349:392–5.
Hyperbaric oxygen therapy may improve symptoms in autistic children 227
[61] Chugani HT, Da Silva E, Chugani DC. Infantile spasms. III. Prognostic implications of bitemporal hypometabolism on positron emission tomography. Ann Neurol 1996;39(5): 643–9.
[62] Gillberg C. Brief report: onset of age 14 of a typical autistic syndrome. A case report of a girl with herpes simplex encephalitis. J Autism Dev Disord 1986;16(3): 369–75.
[63] Ghaziuddin M, Tsai LY, Eilers L, Ghaziuddin N. Brief report: autism and herpes simplex encephalitis. J Autism Dev Disord 1992;22(1):107–13.
[64] DeLong GR, Bean SC, Brown FR. Acquired reversible autistic syndrome in acute encephalopathic illness in children. Arch Neurol 1981;38(3):191–4.
[65] Neubauer RA, James P. Cerebral oxygenation and the recoverable brain. Neurol Res 1998;20(Suppl. 1):S33–6.
[66] Sheffield PJ, Davis JC. Application of hyperbaric oxygen therapy in a case of prolonged cerebral hypoxia following rapid decompression. Aviat Space Environ Med 1976;47(7): 759–62.
[67] Astrup J, Symon L, Siesjo BK. Thresholds in cerebral ischemia—the ischemic penumbra. Stroke 1981;12(6): 723–5.
[68] Neubauer RA, Gottlieb SF, Kagan RL. Enhancing ‘‘idling’’ neurons. Lancet 1990;335(8688):542.
[69] Olsen TS, Larsen B, Herning M, Skriver EB, Lassen NA. Blood flow and vascular reactivity in collaterally perfused brain tissue. Evidence of an ischemic penumbra in patients with acute stroke. Stroke 1983;14(3):332–41.
[70] Jacobson I, Harper AM, McDowall DG. The effects of oxygen under pressure on cerebral blood-flow and cere- bral venous oxygen tension. Lancet 1963;18:549.
[71] Kapp JP, Phillips M, Markov A, Smith RR. Hyperbaric oxygen after circulatory arrest: modification of postische- mic encephalopathy. Neurosurgery 1982;11(4):496–9.
[72] Wallace DJ, Silverman S, Goldstein J, Hughes D. Use of hyperbaric oxygen in rheumatic diseases: case report and critical analysis. Lupus 1996;5(1):84.
[73] Holbach KH, Wassmann H, Kolberg T. Improved revers- ibility of the traumatic midbrain syndrome using hyper- baric oxygen. Acta Neurochir (Wien) 1974;30(3–4): 247–56.
[74] Nighoghossian N, Trouillas P, Adeleine P, Salord F. Hyperbaric oxygen in the treatment of acute ischemic stroke. Stroke 1995;26:1369–72.
[75] Kao CH, Wang SJ, Yeh SH. The relationship among the quantitative perfusion-defect indices in Tc-99m HMPAO brain SPECT, IQ test, and involved extremities in children with cerebral palsy due to perinatal asphyxia. Clin Nucl Med 1994;19(4):309–13.
[76] Montgomery D, Goldberg J, Amar M, et al. Effects of hyperbaric oxygen therapy on children with spastic diple- gic cerebral palsy: a pilot project. Undersea Hyperb Med 1999;26(4):235–42.
[77] Riikonen R, Salonen I, Partanen K, Verho S. Brain perfusion SPECT and MRI in foetal alcohol syndrome. Dev Med Child Neurol 1999;41:652–9.
[78] Heuser G, Heuser SA, Rodelander D, Aguilera O, Uszler M. Treatment of neurologically impaired adults and children with ‘‘mild’’ hyperbaric oxygenation (1.3 ATA and 24% oxygen). In: Joiner JT, editor. Hyperbaric oxygenation for cerebral palsy and the brain-injured child. Flagstaff Arizona: Best Publications; 2002. p. 109–15.
[79] Golden ZL, Neubauer R, Golden CJ, Greene L, Marsh J, Mleko A. Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy. Int J Neurosci 2002;112:119–31.
[80] Singh VK, Warren R, Averett R, Ghaziuddin M. Circulating autoantibodies to neuronal and glial filament proteins in autism. Pediatr Neurol 1997;17(1):88–90.
[81] Singh VK, Rivas WH. Prevalence of serum antibodies to caudate nucleus in autistic children. Neurosci Lett 2004;355:53–6.
[82] Vojdani A, O’Bryan T, Green JA, et al. Immune response to dietary proteins, gliadin and cerebellar peptides in children with autism. Nutr Neurosci 2004;7(3):151–61.
[83] Singh VK, Lin SX, Newell E, Nelson C. Abnormal measles- mumps-rubella antibodies and CNS autoimmunity in chil- dren with autism. J Biomed Sci 2002;9:359–64.
[84] Vojdani A, Campbell AW, Anyanwu E, Kashanian A, Bock K, Vojdani E. Antibodies to neuron-specific antigens in children with autism: possible cross-reaction with enceph- alitogenic proteins from milk, Chlamydia pneumoniae and Streptococcus group A. J Neuroimmunol 2002;129: 168–77.
[85] Vojdani A, Pangborn JB, Vojdani E, Cooper EL. Infections, toxic chemicals and dietary peptides binding to lympho- cyte receptors and tissue enzymes are major instigators of autoimmunity in autism. Int J Immunopathol Pharmacol 2003;16(3):189–99.
[86] Jyonouchi H, Sun S, Le H. Proinflammatory and regulatory cytokine production associated with innate and adaptive immune responses in children with autism spectrum disorders and developmental regression. J Neuroimmunol 2001;120:170–9.
[87] Gupta S, Aggarwal S, Rashanravan B, Lee T. Th1- and Th2- like cytokines in CD4+ and CD8+ T cells in autism. J Neuroimmunol 1998;85:106–9.
[88] Wakefield AJ, Ashwood P, Limb K, Anthony A. The significance of ileo-colonic lymphoid nodular hyperplasia in children with autistic spectrum disorder. Eur J Gastro- enterol Hepatol 2005;17:827–36.
[89] Ashwood P, Anthony A, Torrente F, Wakefield AJ. Spon- taneous mucosal lymphocyte cytokine profiles in children with autism and gastrointestinal symptoms: mucosal immune activation and reduced counter regulatory inter- leukin-10. J Clin Immunol 2004;24(6):664–73.
[90] Torrente F, Ashwood P, Day R, et al. Small intestinal enteropathy with epithelial IgG and complement deposi- tion in children with regressive autism. Mol Psychiatry 2002;7:375–82.
[91] Gupta S. Immunological treatments for autism. J Autism Dev Disord 2000;30(5):475–9.
[92] Zimmerman AW. Commentary: immunological treatments for autism: in search of reasons for promising approaches. J Autism Dev Disord 2000;30(5):481–4.
[93] Akin ML, Gulluoglu BM, Uluutku H, et al. Hyperbaric oxygen improves healing in experimental rat colitis. Undersea Hyperb Med 2002;29(4):279–85.
[94] Luongo C, Imperatore F, Cuzzocrea S, et al. Effects of hyperbaric oxygen exposure on a zymosan-induced shock model. Crit Care Med 1998;26(12):1972–6.
[95] Sumen G, Cimsit M, Eroglu L. Hyperbaric oxygen treat- ment reduces carrageenan-induced acute inflammation in rats. Eur J Pharmacol 2001;431:265–8.
[96] Warren J, Sacksteder MR, Thuning CA. Therapeutic effect of prolonged hyperbaric oxygen in adjuvant arthritis of the rat. Arthritis Rheum 1979;22(4):334–9.
[97] Tokar B, Gundogan AH, Ilhan H, Bildirici K, Gultepe M, Elbuken E. The effects of hyperbaric oxygen treatment on the inflammatory changes caused by intraperitoneal meconium. Pediatr Surg Int 2003;19:673–6.
[98] Chen SY, Chen YC, Wang JK, et al. Early hyperbaric oxygen therapy attenuates disease severity in lupus-prone
228
Rossignol and Rossignol
[99] [100] [101]
[102] [103]
[104]
[105] [106]
[107]
[108] [109] [110] [111] [112]
[113] [114]
[115]
autoimmune (NZB X NZW) F1 mice. Clin Immunol 2003;108:103–10. Buchman AL, Fife C, Torres C, Smith L, Aristizibal J. Hyperbaric oxygen therapy for severe ulcerative colitis. J Clin Gastroenterol 2001;33(4):337–9.
James SJ, Cutler P, Melnyk S, et al. Metabolic biomarkers of increased oxidative stress and impaired methylation capac- ity in children with autism. Am J Clin Nutr 2004;80:1611–7. Sogut S, Zoroglu SS, Ozyurt H, et al. Changes in nitric oxide levels and antioxidant enzyme activities may have a role in the pathophysiological mechanisms involved in autism. Clin Chim Acta 2003;331:111–7.
McGinnis WR. Oxidative stress in autism. Altern Ther Health Med 2004;10(6):22–36. Feldmeier J, Carl U, Hartmann K, Sminia P. Hyperbaric oxygen: does it promote growth or recurrence of malig- nancy? Undersea Hyperb Med 2003;30(1):1–18.
Shaw FL, Handy RD, Bryson P, Sneyd JR, Moody AJ. A single exposure to hyperbaric oxygen does not cause oxidative stress in isolated platelets: no effect on super- oxide dismutase, catalase, or cellular ATP. Clin Biochem 2005;38:722–6.
Yatsuzuka H. Effects of hyperbaric oxygen therapy on ischemic brain injury in dogs. Masui 1991;40(2):208–23. Zamboni WA, Roth AC, Russell RC, Nemiroff PM, Casas L, Smoot EC. The effect of acute hyperbaric oxygen therapy on axial pattern skin flap survival when administered during and after total ischemia. J Reconstr Microsurg 1989;5(4):343–7.
Ozden TA, Uzun H, Bohloli M, et al. The effects of hyperbaric oxygen treatment on oxidative and antioxi- dants levels during liver regeneration in rats. Tohoku J Exp Med 2004;203:253–65.
Yasar M, Yildiz S, Mas R, et al. The effect of hyperbaric oxygen treatment on oxidative stress in experimental acute necrotizing pancreatitis. Physiol Res 2003;52:111–6. Kaelin CM, Im MJ, Myers RA, Manson PN, Hoopes JE. The effects of hyperbaric oxygen on free flaps in rats. Arch Surg 1990;125(5):607–9.
Dennog C, Radermacher P, Barnett YA, Speit G. Antiox- idant status in humans after exposure to hyperbaric oxygen. Mutat Res 1999;428:83–9. Yu SY, Chiu JH, Yang SD, et al. Preconditioned hyperbaric oxygenation protects the liver against ischemia-reperfu- sion injury in rats. J Surg Res 2005;128:28–36.
Alleva R, Nasole E, Di Donato F, Borghi B, Neuzil J, Tomasetti M. a-Lipoic acid supplementation inhibits oxi- dative damage, accelerating chronic wound healing in patients undergoing hyperbaric oxygen therapy. Biochem Biophys Res Commun 2005;333(2):404–10.
Dennog C, Gedik C, Wood S, Speit G. Analysis of oxidative DNA damage and HPRT mutations in humans after hyper- baric oxygen treatment. Mutat Res 1999;431:351–9. Benedetti S, Lamorgese A, Piersantelli M, Pagliarani S, Benvenuti F, Canestrari F. Oxidative stress and antioxi- dant status in patients undergoing prolonged exposure to hyperbaric oxygen. Clin Biochem 2004;37:312–7.
Chavko M, Harabin AL. Regional lipid peroxidation and protein oxidation in rat brain after hyperbaric oxygen exposure. Free Radic Biol Med 1996;20(7):973–8.
[116]
[117]
[118] [119] [120]
[121]
[122] [123]
[124] [125]
[126]
[127] [128]
[129] [130] [131] [132]
[133]
Wada K, Miyazawa T, Nomura N, Nawashiro H, Shima K. Preferential conditions for and possible mechanisms of induction of ischemic tolerance by repeated hyperbaric oxygenation in gerbil hippocampus. Neurosurgery 2001;49:160–7.
Hink J, Jansen E. Are superoxide and/or hydrogen peroxide responsible for some of the beneficial effects of hyperbaric oxygen therapy? Med Hypotheses 2001;57(6):764–9. Barja G. Oxygen radicals, a failure or a success of evolution? Free Radic Res Commun 1993;18(2):63–70. McCord JM. The evolution of free radicals and oxidative stress. Am J Med 2000;108:652–9.
Patel V, Chivukula IV, Roy S, et al. Oxygen: from the benefits of inducing VEGF expression to managing the risk of hyperbaric stress. Antioxid Redox Signal 2005;7(9-10): 1377–87.
Pablos MI, Reiter RJ, Chuang JI, et al. Acutely adminis- tered melatonin reduces oxidative damage in lung and brain induced by hyperbaric oxygen. J Appl Physiol 1997;83:354–8.
Pelaia P, Rocco M, De Blasi RA, et al. Assessment of lipid peroxidation in hyperbaric oxygen therapy: protective role of N-acetylcysteine. Minerva Anestesiol 1995;61(4):133–9. Hollis AL, Butcher WI, Davis H, Henderson RA, Stone WL. Structural alterations in retinal tissues from rats deficient in vitamin E and selenium and treated with hyperbaric oxygen. Exp Eye Res 1992;54(5):671–84.
Boadi WY, Thaire L, Kerem D, Yannai S. Effects of dietary factors on antioxidant enzymes in rats exposed to hyper- baric oxygen. Vet Hum Toxicol 1991;33(2):105–9. Weber CA, Duncan CA, Lyons MJ, Jenkinson SG. Depletion of tissue glutathione with diethyl maleate enhances hyperbaric oxygen toxicity. Am J Physiol 1990;258(6 Pt 1): L308–12.
Thom SR, Bhopale VM, Velazquez OC, Goldstein LJ, Thom LH, Buerk DG. Stem cell mobilization by hyperbaric oxygen. Am J Physiol Heart Circ Physiol 2005; in press. Steindler DA, Pincus DW. Stem cells and neuropoiesis in the adult human brain. Lancet 2002;359:1047–54.
Harch PG, Small T. Interview with Dr. Paul Harch: the application of hyperbaric oxygen therapy in chronic neurological conditions. Medical Veritas 2005;2:637–46. Collet JP, Vanasse M, Marois P, et al. Hyperbaric oxygen for children with cerebral palsy: a randomised multicentre trial. Lancet 2001;357:582–6.
Marois P, Vanasse M. Letter to the editor: ‘‘Hyperbaric oxygen therapy and cerebral palsy’’. Dev Med Child Neurol 2003;45:646–8. Autism Research Institute. Autism Treatment Evaluation Checklist (ATEC) Internet Scoring Program, http:// www.autismeval.com/ari-atec/ [accessed 25.01.06]. Rellini E, Tortolani D, Trillo S, Carbone S, Montecchi F. Childhood autism rating scale (CARS) and autism behavior checklist (ABC) correspondence and conflicts with DSM-IV criteria in diagnosis of autism. J Autism Dev Disord 2004;34(6):703–8.
Constantino JN, Davis SA, Todd RD, et al. Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J Autism Dev Disord 2003;33(4):427–33.
m

Get Informed!
Please take a moment and request more information on how Hyperbaric Oxygen Therapy can improve the quality of your life today!Stem Cell Therapy
Testimonies
- Jimmy V. Calcagno
We miss all of you there, too. Maybe we'll get back to you some day. You made us feel very comfortable. I feel a lot better already, and can't wait to get back bowling. I start today. Wish me luck. Regards to all and GOD BLESS YOU. Vincent ( Jim ) and JO - Cherie Alvis
My experience in the hyperbaric Chamber was an easy and pleasant time. Very friendly professional staff. The office hours were great, because it was really conducive for my schedule. - Mary, Colorado Springs
I have relied on the experts that are opening Hyperbaric Centers of Florida to provide treatment for my Lyme Disease for the past five years. - Debbie, Oklahoma City
Six years ago I was given four months to live as a result of liver failure. The owners of Hyperbaric Centers of Florida provided treatment for me at their center in Texas and I was able to begin to grow new liver tissue. My primary care physician can not believe that his four month prediction was incorrect. I do require "booster therapy" which involves a few treatments every 6 to 8 months, but my health is excellent and I look forward to a long and productive life.